I would like to begin by acknowledging/pointing out two things.
FIRST – It’s been estimated that something like 35% of all medicines currently being used had their origins in plants.
SECOND – Up until the turn of the 20th century, the average life expectancy was about 40 years – somewhat longer, if you made it through childhood.
To me, if you take those two facts, what you end up with is a conclusion that while plants have biologically active substances in them (in other circles, these substances are sometimes referred to as “drugs”), however, people really hadn’t harnessed those substances during the first 200,000 so years of the existence of Homo sapiens. Horses still haven’t figured it out.
So, why the rush (in some circles) to give plants and herbs to horses?
The available scientific evidence on individual herbal medicines in people is sometimes considered “promising.” However, only very rarely is their convincing evidence, or evidence that is considered sufficient to make a sound clinical decision for prescribing them. Most studies or reviews of studies show that the reported effects of herbal products seem to be rather limited, or need further confirmation by well-designed trials, or both. In addition, data that directly compares herbal remedies with well-established pharmaceutical products are often not available or do not provide much useful information (for example, data may be derived from studies that failed to include a placebo group).
A basic problem concerning all clinical research in herbal medicines is the question of whether different products, extracts, or even different lots of the same extract are comparable and equivalent. For example, echinacea products may contain other plant extracts, use different plant species, different parts of the plant (herb, root, both), and might have been produced in quite different manners. In addition, the concentration of active ingredients can vary dramatically depending on where the plants were grown or when they were harvested. Finally, even a claim of “standardization” does not mean the preparation is accurately labeled, nor does it indicate less variability in concentration of constituents of the herb. Therefore, any given bottle of an herb may contain different amounts of any active substance from those contained in another bottle of the same herb.
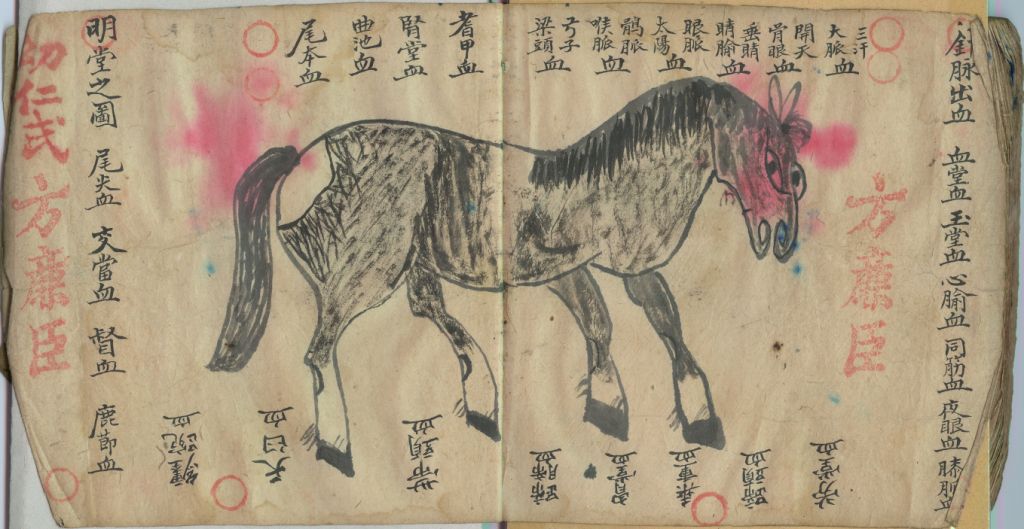
Such inherent variation in products means that it may not be possible to extrapolate the results of any one study to any particular product. And, of course, almost all of the trials of individual herbal products have been done in people; applying the findings of individual trials in human medicine to horse care is problematic because of the fact that different species may react to the same substance in different ways.
Herbal products may be prescribed for reasons that diverge from known medical practice. That is, treatments may be prescribed or based on vague rationales for which there is no proof, or which make no sense. For example, observations such as, “underfunctioning of a patient’s systems of elimination” or “an accumulation of metabolic waste products” make no medical sense whatsoever. However, based on such fanciful suppositions, plants with purported diuretic or laxative actions might then be prescribed. Herbal products might also be prescribed to “support” various body systems, even though the term “support“ is vague and ill-defined, there may be no evidence that such systems are in need of support, and there may be no evidence that the prescribed plant supports anything anyway!
Herbal products may also be contaminated, adulterated, or misidentified. For example, in 1998, the California Department of Health reported that 32 percent of Asian patent medicines sold in that state contained undeclared pharmaceuticals or heavy metals; this appears to be a particular problem in herbal preparations from Asian sources. Outright fraud also exists; in 2003, The Australian Therapeutic Goods Administration (TGA) suspended the license held by Pan Pharmaceuticals Limited of Sydney to manufacture medicines because of serious concerns about the quality and safety of products manufactured by the company. Because of such problems, calls for tighter regulation of botanical medicines have appeared.
Controlled studies on the clinical effects of herbal or botanical preparations in horses are virtually non-existent. It’s usually not known how the doses are obtained; they are often “proportional” to those used in human herbal medicine. However, it should be kept in mind that experience with pharmaceuticals has shown that extrapolating dosage or toxicity data from one species to another can be dangerous. Due to their inherent toxicity, some herbal remedies, such as belladonna, should probably not be used in horses under any circumstance. Others, such as tea tree oil, while generally safe at some strengths, can cause significant adverse effects at others. In addition, because some herbal remedies contain multiple, biologically active constituents, interaction with conventional drugs is also a concern. Just because herbal products may be “natural” doesn’t also mean that they are safe; rattlesnake bites and hurricanes are “natural,” too!
While science continues to demonstrate that there are biologically active substances in plants, the fact is that those substances are best administered when they are identified, and standardized. Yew trees contain an anti-cancer agent; it wasn’t until Tamoxifen® was purified that the active ingredient became useful. There’s no good reason to give your horse substances of unknown purity, with unknown effectiveness. It’s just a waste of time and money.